Abstract
Seventy percent of all patients with light chain amyloidosis (AL) have cardiac involvement, and most of those patients ultimately die from complications related to their heart disease. While consensus guidelines outline criteria for grading hematologic response to chemotherapy for AL, there are no currently validated criteria for grading cardiac response to therapy. Recently, Muchtar et al. created a system for grading organ response, but excluded previously treated patients and those requiring multiple lines of therapy to achieve a response. Because the majority of AL patients receive multiple lines of therapy during their treatment course, we sought to validate cardiac grading criteria and demonstrate that they can be applied to a heterogeneous group of patients, including those who have been treated previously. Here we show how depth of best cardiac response at any point during a treatment course predicts both overall survival and risk of subsequent cardiac relapse defined as progression after an initial cardiac response.
This is a retrospective cohort study of patients followed at the Stanford Amyloid Center with underling plasma cell dyscrasias causing biopsy-proven systemic AL involving the heart. Grading cardiac response involves categorizing the best response (the lowest NT-proBNP value) after initiation of treatment as either no response (NR), partial response (PR), very good partial response (VGPR), or complete response (CR). PR and VGPR are defined as a >30% and >60% reduction in NT-proBNP respectively; CR is defined as NT-proBNP<450 pg/mL. Per consensus guidelines, cardiac progression is defined as a >30% and >300 ng/L increase in NT-proBNP, whereas NR does not meet response criteria requiring a >30% and >300 ng/L reduction in NT-proBNP. Survival times were calculated from the time of first treatment to patient death or end of study (January 2018).
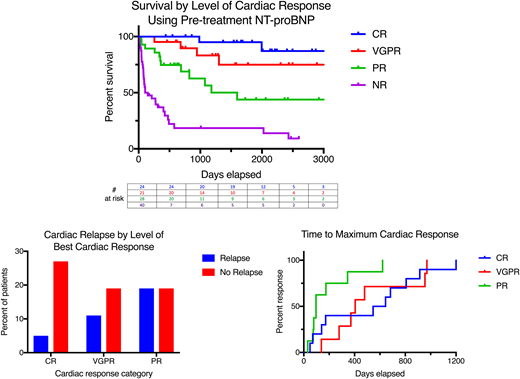
Out of 252 patients with cardiac AL treated between June 2007 and January 2018, 114 had sufficient data for evaluation. Of those, 74 patients (65%) had cardiac responses to treatment, and 40 (35%) did not demonstrate a cardiac response. Of the responders, 60% had received more than one line of therapy by the time they achieved their best cardiac response. Kaplan Meyer survival analyses of patients grouped by cardiac response to therapy reveal that best depth of cardiac response to therapy at any point during the treatment course is predictive of overall survival by the log-rank test using a pre-treatment NT-proBNP assessment (p<0.0001). Patients who achieve CR have a 5-year overall survival of 96% compared to 74% for VGPR, 43% for PR, and 13% for NR. Results of a landmark analysis using NT-proBNP values after 6 months of treatment yielded the same statistically significant result (p<0.0001). A subset analysis of patients who required multiple lines of therapy to achieve their best cardiac response was also significant (p=0.0014). Patients who achieve deeper cardiac responses are also less likely to experience subsequent cardiac relapse (p=0.012), and patients who relapse have less robust percent reductions in NT-proBNP than those who do not (p=0.0017). For example, 5% of responders in our cohort achieved a CR and subsequently experienced a cardiac relapse, as compared to 11% of VGPR patients and 19% of PR patients. Additionally, deeper cardiac responses take longer to achieve that shallower responses (p=0.027). Median time to response for CR patients is 595 days, as compared to 405 days for VGPR patients and 96 days for PR patients. Depth of hematologic response is significantly associated with cardiac response (p<0.0001), but not with cardiac relapse (p=0.69), while in contrast, hematologic relapse is strongly associated with cardiac relapse (p=0.0002).
Our findings validate cardiac response grading as a useful tool for prognostication. Moreover, we demonstrate that cardiac response grading can be applied to patients who received several lines of therapy. This both increases the applicability of the tool and, in the context of CRs taking longer to achieve, demonstrates the clinical imperative to continue aggressive therapy in patients with suboptimal cardiac responses. Indeed, a CR or even VGPR achieved later in an illness trajectory has a demonstrated overall survival and cardiac progression free survival benefit.
Schrier:Forty Seven Inc.: Consultancy. Liedtke:Amgen/Onyx: Consultancy, Honoraria, Research Funding; BlueBirdBio: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; celgene: Research Funding; Caelum: Membership on an entity's Board of Directors or advisory committees; Prothena: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Genentech/Roche: Research Funding; Gilead: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal